“Health systems and related stakeholders must commit to understanding and integrating the individual, their needs, and the dueling conditions which impact their lives to effectively identify tools and strategies that reduce the tension among providers of care, services, and supports, and allow the whole individual to emerge along a pathway to recovery.”~ Mental Health AmericaFor the last 70 years, each May has been observed in the United States as National Mental Health Month. Originally established in 1949 by the Mental Health America organization, it has become the largest public campaign focused on promoting mental health awareness in the world. In 2018 alone, approximately 30 million people were given up-to-date and relevant information about good emotional and/or behavioral health. More importantly, they were connected with local resources that are available to help them achieve just that.Behavioral and emotional disorders frequently manifest with other physical or mental health conditions. Cooccurring disorders –also called dual diagnosis – can negatively impact a person’s quality of life and even impair their ability to function.For example, a person suffering from chronic pain due to injury or illness may also struggle with depression, which also puts them at greater risk for a Substance Use Disorder – alcoholism, an addiction to illicit drugs, or the misuse of prescription medications.This is why the theme for 2019 is so timely and appropriate: “Dueling Diagnoses: Mental Health and Chronic Conditions in Children in Adults”.
What is A Dual Diagnosis?
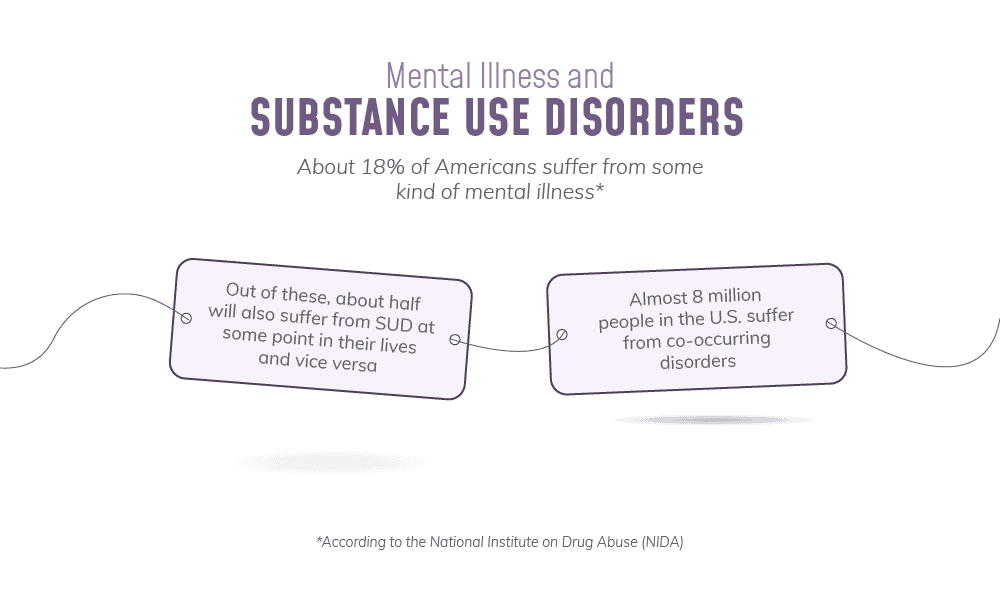
“…each disorder exacerbates the other and also predisposes to relapse in the other. At times, the symptoms can overlap or even mask each other, making diagnosis and treatment all the more difficult.”~Robert B. Pereia, Faces of Dual Diagnosis: A Canadian PerspectiveSimply put, a dual diagnosis is when a person is dealing with one or more mental illness and SUD at the same time. This happens much more than you might think. According to the Epidemiologic Catchment Area (ECA), 44% of patients with psychiatric disorders also struggle with problem drinking and 64% abuse drugs.Sometimes, mental illness will precede substance abuse. A person who is in mental pain will desperately turn to alcohol and drugs for relief. “Self-medicating” is always a bad idea, because substance abuse invariably leads to additional problems that can worsen the original condition.In fact, that is exactly what happens when the addiction comes first. Out-of-control substance abuse results in traumatic experiences and other stresses and negative consequences that can cause or worsen many emotional or behavioral conditions.For example, people who abuse alcohol and/or drugs are more at risk for:
- Injuries – According to the World Health Organization, up to 18% of injuries treated in Emergency Rooms are alcohol-related.
- Accidents – Workers who are problem drinkers are 2.7 more likely to miss work due to injury.
- Car Crashes – The National Highway Traffic Safety Administration reports that in 2016, 10,497 Americans died in alcohol-related wrecks. In addition, marijuana users are at 25% greater risk for a crash than non-users.
- Arrests – 2 out of every 3 male arrestees test positive for alcohol and/or drugs
- Violence – Per the National Institute on Alcoholism and Alcohol Abuse, up to 86% of homicide offenders were drinking at the time of the crime.
- Sexual Assault – 80% of college students who are sexually assaulted were intoxicated at the time.
- Intimate Partner Violence – 92% of assailants were drinking at the time of the incident.
What Mental Disorders Co-Occur with Addiction?
“‘Sanity’ was not something I was particularly familiar with. I have mental illness, bipolar disorder, and that in itself had taken from me time and time again the sanity I desperately wanted. Compounded by years of the insanity of alcoholism and addiction, I was, at that time, pretty well convinced that sanity was something that I could never hope for.”~ Marya Hornbacher, Sane: Mental Illness, Addiction, and the 12 StepsSUD and mental illness share many causal and environmental and genetic factors, and their co-occurrence surprisingly often:
Post-Traumatic Stress Disorder: Present in 70% of People with SUD
While psychological trauma is characterized by disruptions in a person’s sense of control, addiction can also be viewed as a disorder of control, or more accurately, an inability to control. The loss of control is insidious, often unrecognized by the addict until, in Alcoholics Anonymous terms, life becomes unmanageable.”~Psychological Trauma and Addiction Treatment, edited by Dr. Bruce Carruth, Ph.D., LCSWSevere unresolved trauma can result in painful feelings that are difficult to process. A person who has not dealt with these issues may often turn to intoxicants. They do this for two primary reasons:
- To numb emotional or physical pain.
- To escape from or forget about the negative emotions and uncomfortable memories they associate with the past trauma.
Substance abuse is a very common unhealthy coping mechanism for many people with a mental illness.
Depression: 67%
“But like all destructive behaviors that keep you from going inward and doing the hard work, booze turned on me. The stuff to which I attributed my social grace, beauty, and intelligence was nothing but a backstabber that ultimately brought me to a place where I cried uncle and asked God to take over.”~ Therese Borchard, Beyond Blue: Surviving Depression & Anxiety and Making the Most of Bad GenesDepression and addiction each worsen the other. Alcoholics and addicts experience unpleasant consequences that impact their peace of mind and self-esteem, often resulting in depression. Substance abuse also changes the brain, resulting in:
- Poor decision-making
- Memory problems
- Confusion
- Difficulty in concentrating
- Impaired impulse control
- Unpredictable mood swings
- Cognitive decline
These issues can each contribute to the development or worsening of a depressive disorder.
Bipolar Disorder: 60%
“The biggest problem alcohol use poses for people with bipolar is how it interacts with moods.”~ Dr. Henry R. Kranzler, MD, Professor of Psychiatry and Director of the Center for Studies of Addiction, University of PennsylvaniaThe depressive lows and manic highs that characterize BPD makes life difficult for its sufferers.When they are UP (manic cycle), the person will feel creative and creative and confident. But they may also have difficulty controlling their impulses, engage in risky behaviors, and suffer from sleep disturbances. And when they are DOWN (depressive cycle), they may lose the ability to experience any pleasure at all. Nothing makes them happy or even content. Worse, become disinterested in the things they used to enjoy—social interaction, hobbies, work, sex, or even eating.As a result, many people with BPD try to contain their symptoms with drugs and alcohol, hoping to dial down their mania and ease their depression.But here’s the truth —substance abuse WORSENS bipolar disorder.
- Marijuana triggers manic episodes
- Stimulants such as methamphetamine and cocaine produce out-of-control highs and debilitating crashes that resemble BPD.
- Opioids and alcohol are depressants.
Anxiety: Approximately One-Third
“The panic attacks, the suicidal thoughts, all come at once and there’s not much you can do about it really. Alcohol has played a big part. I know it’s a trigger…The majority of panic attacks and manic-depressive stages come after a drinking session. It’s a downward spiral…I was really socially anxious. I’d have to get exceptionally drunk just to feel like I wasn’t out of place. It’s like alcohol is the way out, but I know it isn’t – it just makes things 20 times worse.”~ Mat, “My Mind and Me”Alcohol is a Central Nervous System depressant that slows respiration and heart rate and lowers blood pressure, so you might naturally expect that it has a calming effect on someone struggling with anxiety. That is why they frequently might start drinking when they start experiencing symptoms.But oddly enough, alcohol tends to make anxiety even worse, in at least six identifiable ways
- Central Nervous System – Although alcohol is a sedative, it triggers hyperactivity in some people, as their body tries to counteract that sedation. Some of the side-effects of hyperactivity include insomnia, tremors, and a sensitivity to light.
- Mood – Alcohol abuse reduces the amount of serotonin in the brain. Serotonin is one of the neurotransmitters associated with learning, reward, and feelings of happiness. Serotonin deficiency worsens anxiety.
- Concentration – Being intoxicated – poor concentration, confusion, and lowered inhibitions –results in impaired judgment, frustration, and anxiety.
- Low Blood Sugar—Drinking triggers insulin production in the pancreas, which in turn causes blood sugar levels to fall. Symptoms of low blood sugar include dizziness, confusion, shaking, and nervousness.
- Heart Rate – Alcohol does slow the heart rate, but it is also a vasodilator, meaning it opens blood vessels. So the immediate effect is a faster heartbeat. This resembles heart palpitations and can increase anxiety.
- Dehydration – The symptoms of dehydration – weakness, lightheadedness, dizziness, nausea – can cause the person to feel so unwell that their anxiety increases.
Disordered Eating: Quintupled Risk of Substance Abuse
“No matter what we weigh, those of us who are compulsive eaters have anorexia of the soul. We refuse to take in what sustains us. We live lives of deprivation. And when we can’t stand it any longer, we binge. The way we are able to accomplish of this is by the simple act of bolting – of leaving ourselves – hundreds of times a day.”~ Geneen Roth, Women, Food, and God: An Unexpected Path to Almost EverythingAmong people with an eating disorder, the rate of SUD is five times higher than that of the general population. One theory about this frequent comorbidity is shared neurotransmitters that may influence either condition.
- Some abused substances, such as meth or coke, suppress the appetite and support certain eating disorders.
- A side-effect of excessive drinking is nausea and vomiting, which supports “binging and purging”.
In a general way, both disordered eating and SUD are striking alike. Both are:
- Characterized by a compulsive loss of control.
- Can involve excessive consumption.
- Cause and be caused by overwhelming anxiety, depression, shame, guilt, anger, powerlessness, self-loathing, feelings of worthlessness, or other emotional pain.
The unhealthy activity – the drinking or the disordered eating – triggers a release of pleasure-causing endorphins that “train” the brain that the activity is good, necessary for survival, and worthy of repeating. This supports continued illness.
Schizophrenia: 1000% More Likely to Use Drugs or Drink
“There is growing consensus that cannabis use might increase the risk of developing schizophrenia. Our results support this, but also suggest that those at increased risk of schizophrenia may be more likely to try cannabis in the first place.”~ Professor Marcu Munafo, Bristol University’s School of Experimental PsychologyPeople who either have or are predisposed to schizophrenia are far more likely to use drugs and alcohol than the general population. 45% of schizophrenics will develop SUD during their lifetime, and 14 are addicted right now.Take a look at the drug usage rates among people with schizophrenia:
- Cigarettes: Up to 90%
Compared to non-smokers, daily smokers are twice as likely to develop schizophrenia, and their symptoms manifest a year sooner. Of special relevance, schizophrenics have a life expectancy that is 25 years shorter, chiefly due to smoking-related illnesses.
- Alcohol: 65%
Long-term heavy drinking can lead to alcohol-induced psychosis. This condition can mask the symptoms of still-developing schizophrenia, delaying early diagnosis and treatment. Schizophrenics who drink may be more prone to anger, aggression, violence, and hallucinations.
- Marijuana: 51%
40% of marijuana user exhibit symptoms of schizophrenia. Heavy cannabis use before the age of 18 increases the risk of schizophrenia within 15 years by 600%.
- Cocaine: 23%
Because it impairs attention and memory, cocaine abuse increases anxiety, deepens depression, and worsens the social anxiety that schizophrenics suffer.
- Opioids: 4%
Schizophrenics who abuse heroin or prescription painkillers are hospitalized at a 45%higher rate than those who use amphetamines and over 80% more often than those who smoke marijuana.
- Methamphetamine
Compared to those who abuse opioid, cocaine, or alcohol, people who use meth have a tripled risk of developing schizophrenia.
Why Is 2019’s Theme So Important to Substance Abusers?
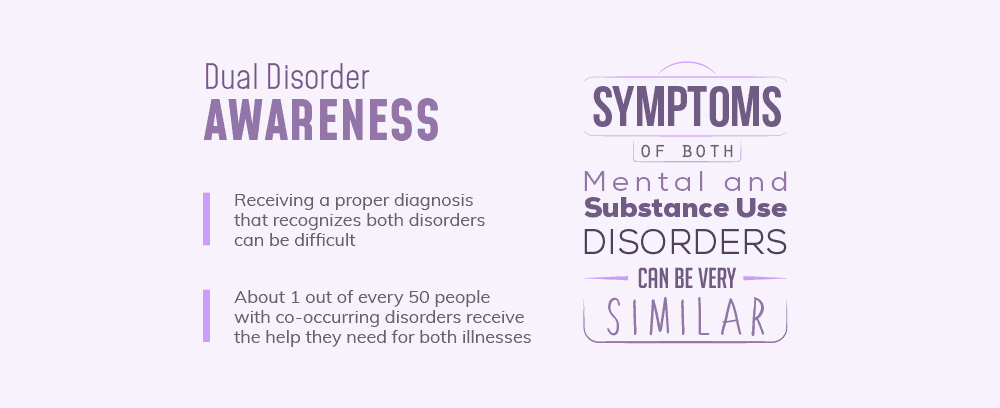
“In deciding this theme, we were thoughtful in characterizing the diagnoses themselves as “dueling,” because once a condition is diagnosed, it often becomes not just the primary diagnosis for health care providers, but the primary lens through which that individual is seen. And when a second condition is observed, there is often unnecessary tension among the providers, the individual and sometimes their family, as to what diagnosis takes precedence and who should take the lead in organizing and managing care and support.”~ Mental Health AmericaBecause many of the symptoms of addiction and mental illness resemble each other, receiving a proper diagnosis that recognizes both disorders can be difficult. In fact, doctors and mental health providers who do not specialize in dual diagnoses can often fail to address all of the patient’s needs.This is why only about 1 out of every 50 people with co-occurring disorders receive the help they need for both illnesses. 2019’s theme for Mental Health Awareness Month suggests several extremely-effective, but often-underused strategies that, when used properly, can promote improved mental health and general wellness.
Humor: Truly One of the Best Medicines
“Please Lord, teach us to laugh again, but, God, don’t let us ever forget that we cried.”~ Meiji Stewart, Keep Coming Back: Humor and Wisdom for Living and Loving RecoveryLaughter has many benefits that can support successful recovery, including:
- Decreases levels of stress hormones
- Activates the reward system of the brain
- Causes the release of endorphins, which are known as natural pain blockers
- Improves overall mood
- Reduces anxiety
- Alleviates depression
So how can someone in recovery for a dual diagnosis incorporate humor into their life?
- Watch funny movies and television shows.
- Don’t forget about cartoons. There’s nothing wrong with rediscovering the innocent joy you had as a child.
- Practice telling jokes.
- Get together often with positive friends.
- Go to 12-Step meetings as often as you can. You will always find “old-timers” who have managed to find the humor in their situations.
- Most of all, remember that you don’t have to take yourself so seriously all the time.
Religion and Spirituality
“Spirituality is experiencing our own personal power, experiencing the confidence of knowing we have the power to bring every good feeling into our lives, a power that is not paranoid or selfish. It is not cruel, prideful, or unworthy, but appreciates the abilities and individual gifts that we have all been given.~ Leo Booth, Spirituality and Recovery: A Classic Introduction to the Difference Been Spirituality and Religion in the Process of HealingRegular spiritual practice and personal religious beliefs profoundly affect body chemistry and brain activity:
- Higher levels of dopamine, endorphins, and serotonin
- Lower levels of stress hormones such as noradrenaline or cortisol
- Devout people who read the Bible experience increased activity in the regions of the brain associated with reward and positive feelings.
- Regular attendees at religious services have a rate of depression that is over 20% lower than those who do not attend.
- Among depression patients, 80% report that religion helps them cope with life.
- 65% use religion to cope with the severity of their symptoms.
- 30% report that their religion gives them a reason to live.
Support Animals and Pets
“The evidence is overwhelming that animals make us happier, healthier, and more sociable…”~ Dr. Aline Kidd, Department of Psychology, Mills College, speaking to the American Association for the Advancement of ScienceThe companionship of animals has a profoundly positive impact on their owner’s quality of life by giving trust, freedom from judgment, and unconditional love.
- 8 in 10 of owners say that their pet provides emotional support and makes them happy.
- 2 in 3 think that their pet reduces their stress.
- 55% believe that their pet alleviates their anxiety and depression.
There are several ways to enjoy this closeness – keeping a pet, participating in pet/equine therapy, or obtaining an emotional support animal.
Recreation and Social Connections
“No person, trying to take responsibility for her or his identity, should have to be so alone. There must be those among whom we can sit down and weep, and still be counted as warriors.”~ Adrienne Rich, SourcesDoing those healthy things that bring you pleasure and finding supportive friends to relate to are both crucial to recovery from addiction and good mental health:
- A strong social or personal support system helps with recovery from stress.
- It also leads to improved treatment outcomes.
- Vacations reduce stress and improve happiness.
- Teens and adolescents who participate in sports—which boost self-esteem and sociability—have a lowered risk of depression and suicide.
- Leisure activities such as dancing, playing board games with others, playing musical instruments, and reading reduces the risk of dementia.
A Healthy Work-Life Balance
“Workaholism is the best-dressed problem of the twenty-first century. Workaholics often have comfortable incomes, and their families appear to have all the material comforts…But behind closed doors, workaholics are breaking down inwardly, and their families suffer in quiet desperation.”~ Dr. Bryan E. Robinson, Chained to the Desk: A Guidebook for Workaholics, Their Partners and Children, and the Clinicians Who Treat ThemWhen your job takes over the rest of your life, it can cause serious damage to your mental and physical health. distressingly, nearly 40% of American adults work 50 or more hours per week, and almost 20% put in at least 60 hours.Too many don’t even take advantage of one of their workplace benefits. According to the Economic Policy Institute of Washington, D.C., 36% of U.S. workers do not intend to use their full vacation. The mindset is, “We have to get ahead of our workload in order to leave, and then we have to catch up to our workload upon our return.”Of concern, over half of respondents to a recent survey admit that they cope with workplace stress in an unhealthy manner – using drugs or drinking, for example. Approximately 75% of employees feel that their job/career will suffer if they take time off to focus on their mental health.Addiction, mental illness, and workaholism are closely linked:
- Many recovering addicts struggle to find new outlets for the energy and time that they used to devote to substance abuse. Some throw themselves completely into their work, thinking that it is a positive obsession.
But when professional success means personal failure, all they have done is swap one addiction for another.
- Workaholics tend to be awkward in non-work situations. This takes away the social support they need for sobriety and balance.
- Workaholics often struggle to make personal connections with others, leaving them feeling and isolated.
- Workaholics are frequently poor communicators, making it hard for them to express their emotional needs.
- All of this explains why workaholics have such high rates of depression and suicide.
By healthy work-life balance results in:
- Greater job satisfaction
- Increased feelings of contentment and happiness
- Reduced stress
- Fewer symptoms of depression or anxiety
- More time for recreation and social interaction
- Opportunities for personal bonding with family and friends.
Professional Help for a Dual Diagnosis
The “standard” treatment offered by most mental health providers or rehab programs simply is not sufficient to truly help someone with a dual diagnosis. Unfortunately, most addiction recovery programs don’t adequately address co-occurring mental illness, and very few counselors and therapists have sufficient adequate resources to properly deal with active addiction.But this invariably means that one condition gets treated before the other. Not only does this complicate recovery, it sets the stage for relapse.The National Alliance on Mental Illness advises that for treatment to be successful, both conditions should be treated at the same time, with both regarded as the primary disorder. An individualized treatment plan might include some combination of:
- One-on-one behavioral counseling
- Education about addiction and mental illness
- Peer group therapy
- Proper nutrition
- Exercise
- Healthy coping methods
- Improving communication
- Avoiding triggers
- Relapse prevention and response
- Exercise
- Recreational therapy
- Art or Poetry therapy
- Animal or Equine Therapy
- Support or fellowship groups
- FDA-approved medications
- Family education and services
- Long-term aftercare
Top dual diagnosis rehab programs have each service provider working together as a team. This integrative and comprehensive approach means that all of your recovery needs are handled by a clinical staff sharing the same treatment goals and philosophy.
What Does All of This Mean to YOU?
The biggest takeaway from all this information is that if you are like the millions of Americans who struggle with either substance abuse or a mental disorder, you should also be aware that it is very likely that you actually need help for BOTH. You need a thorough evaluation from a specialist.Next, you should understand that you cannot find the help you need just anywhere. Because all recovery programs are not created equal, you need to find a program specifically designed to help people with a dual diagnosis. In fact, that should be one of the first questions you ask.National Mental Health Awareness Month is the ideal time to do what is best for you, your emotional well-being, and your future. With the help of the program that uses an evidence-based approach to address both the addiction and the mental illness, you can successfully regain your sobriety and your balance, and finally, become the best version of YOU possible.
What Did you Think About This Blog?
Give it a Rating!