“A chat with the Grim Reaper should be enough to scare away any thought of relapse. Wish it were that easy, but not even days conversing with Death can disintegrate the claws of addiction.” ~ Ellen Hopkins, Traffick For anyone attempting to regain their sobriety, one of the most dangerous sayings thrown around is “Relapse is part of recovery.” From some perspectives, that could be seen as giving tacit approval to drink and use drugs again. To be perfectly clear—substance abuse during recovery from addiction is NEVER okay. The nature of the disease of addiction means that there are no guarantees. In fact, resuming drug use after a period of sobriety greatly increases the likelihood of a fatal overdose. This what happened in the tragic deaths of actors Cory Monteith and Philip Seymour Hoffman. Perhaps a better way to phrase it is “Relapse is part of the DISEASE.” With that adjusted mindset, we can more appropriately look at how to (a) take steps to prevent relapse, and (b) properly respond and continue moving forward in recovery if a relapse does occur.
“Get the help you need today. We offer outpatient assistance, so you can maintain your work, family, and life commitments while getting the help you deserve!”
Is Relapse Inevitable?
“And the greatest difficulty is that it’s not the elbow that becomes addicted, but the brain. The very origin that likes alcohol is trying to determine whether to change the behavior. Guess what it will always decide?” ~ Bert Pluymen, The Thinking Person’s Guide to Sobriety But even though a person in recovery should do everything possible to safeguard their sobriety, the insidious nature of addiction means that relapse is an unfortunate reality for far too many. It is not exactly an inevitability, but it is a distinct possibility that should be prepared for.
Relapse Statistics
“Relapse is about the return to an active disease process following a period of recovery from that disease process. One very important fact…you can’t relapse in any disease until you’ve been in recovery from it. This is the truth in any illness. If someone has not yet got into the recovery process, they CANNOT have a relapse.” ~ Linda Free-Gardiner, Trust the Process: How to Enhance Recovery and Prevent Relapse The National Institute on Drug Abuse defines addiction as a “chronic, relapsing brain disease”. This means it is a lifelong condition that can manifest as dangerous flare-ups—i.e., relapses—if not treated properly. As with all chronic illnesses, personal behavior is critical to successful management. But this also means that sometimes, people will not fully comply with their recommended plan. For example, a patient with diabetes might eat too many sweets and fail to lose excess weight. Or perhaps a person with high blood pressure will keep smoking. Likewise, someone with an addictive disorder can slip or relapse. For comparison purposes, here are the relapse/nonconformance rates of various illnesses:
- Substance Abuse Disorder: 40%-60%.
- Type II Diabetes: 30%-50%.
- Hypertension: 50%–70%.
- Asthma: 50%–70%.
- Bipolar Disorder: 50%-70%.
- Depression: 33%-50%.
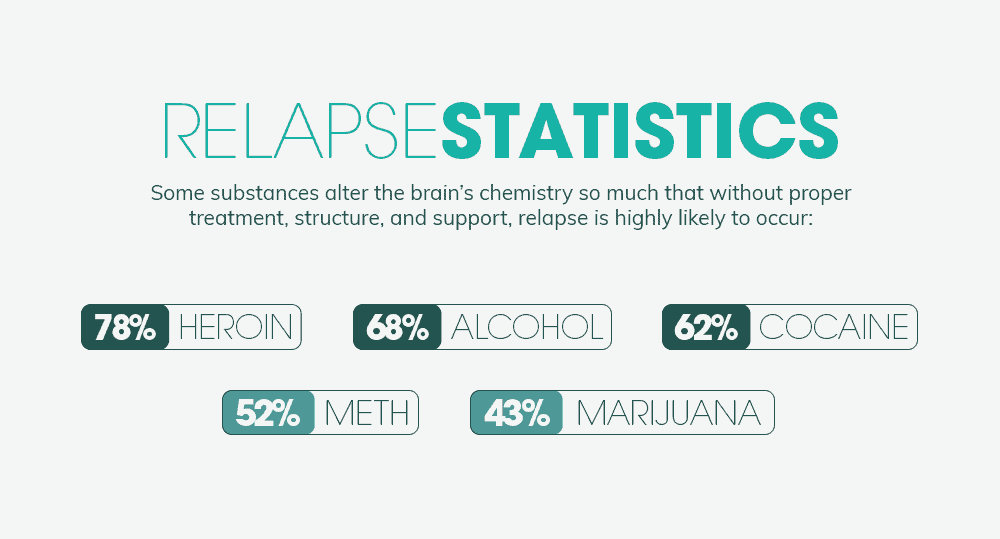
Obviously, noncompliance and relapses are extremely common. Per a 2012 Psychology Today article, up to 90% of people in recovery will experience “at least one mild to moderate slip.” The specific drug of choice also matters. Some substances affect the brain so profoundly that without proper treatment, structure, and support, relapse becomes a probability, rather than a possibility.
- Heroin – 78%
- Alcohol – 68%
- Cocaine – 62%
- Methamphetamine – 52%
- Marijuana – 43%
- Hallucinogens – 42%
Finally, it is important to remember that drug detox – simply getting clean – is NOT rehab, and on its own, it is not an effective way to manage addiction. Additional services are required. In fact, patients who participate in a rehab program within 30 days of completing a detoxification program are 10 times less likely to relapse. Conversely, up to 80% of patients who only detox will relapse.
What is the Difference Between a Slip and Relapse?
“A slip is an error in learning… (People) who recover from habits they want to change treat slips very differently. They see themselves as having made a mistake they needn’t repeat. And RECOVERING from a slip gives them stronger confidence in their ability to resist temptation.” ~ Dr. G. Allan Marlatt, the University of Washington While both “slip” and “relapse” refer to a return to the use of intoxicants after a period of regained sobriety, they are not interchangeable. The primary difference is the duration and the damage.
- A “slip” is when a person in recovery very briefly returns to drinking or drugging. Almost immediately, they realize that they have made a serious mistake, so they quickly resume their program of recovery.
- A “relapse” is considered a more serious and longer-lasting return to active substance use. it means that the person has for the foreseeable future totally abandoned their efforts at recovery.
A relapse may begin as a slip and then quickly worsen. A relapse has the potential to incur serious consequences – illegal behaviors, job loss, violence, overdose, or even a complete abandonment of sobriety. 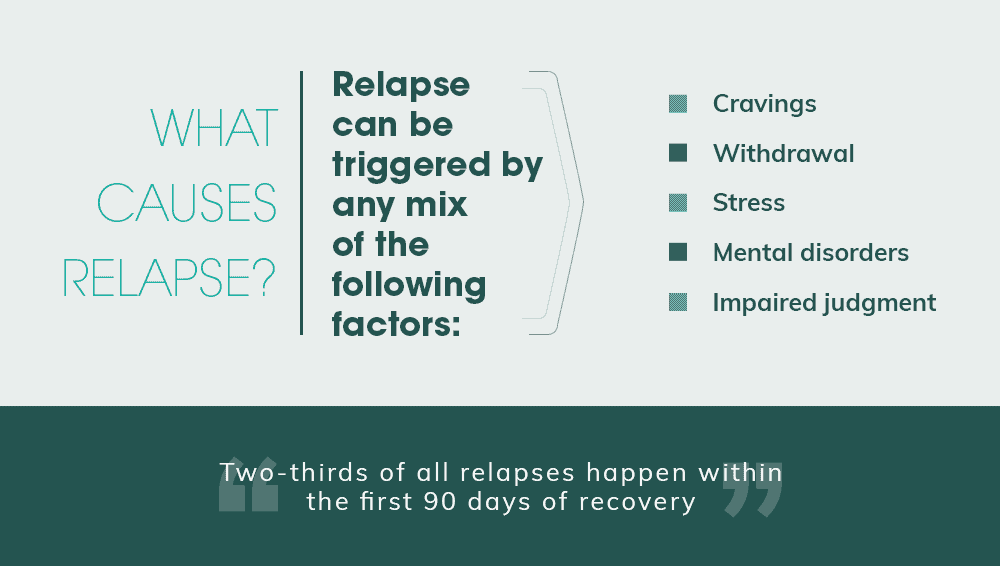
What Causes Relapse?
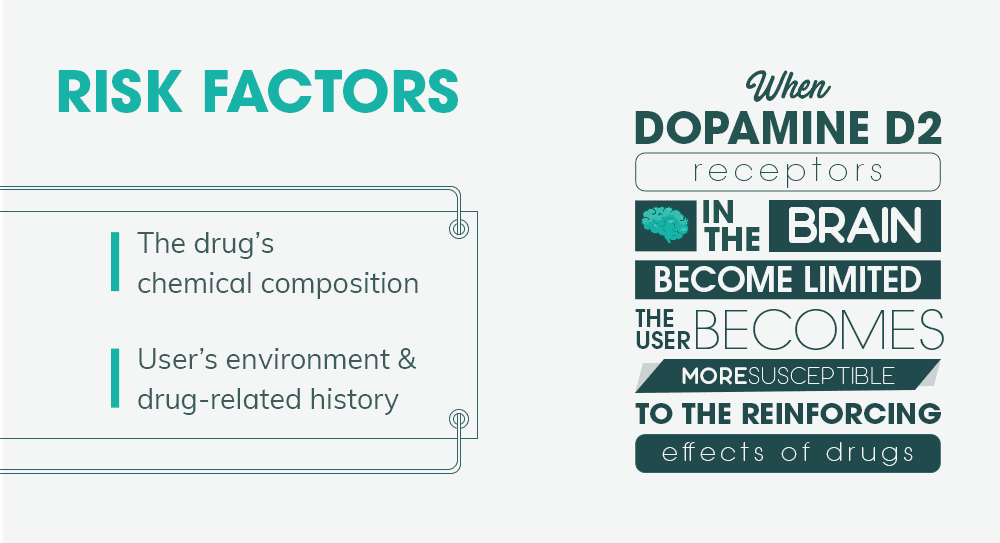
“When a person who has this disease is exposed to cues, or stimuli, that remind them of or previously have been associated with the use of the drug, there is an uncontrollable reflex that happens very, very quickly. The person doesn’t have the ability to stop it. It may happen before they are even conscious of it.” ~ edited by John Hoffman and Susan Froemke, Addiction: Why Can’t They Just Stop? Addiction is a complicated disease, caused and influenced by many factors – genetics, environment, personal habits, co-occurring illnesses, experiential history, etc. Likewise, a relapse may be triggered by any or all of the following causes:
- Cravings – The physical and mental compulsion to abuse alcohol and drugs.
- Withdrawal – Painfully-uncomfortable symptoms that manifest when the substance discontinued.
- Stress – Often, intoxicants are used as a coping method whenever the pressures of everyday life become overwhelming. Until a person acquires new, healthier coping mechanisms, they will feel a “need” every time they face difficulties.
- Drug cues – The people, places, and things formally associated with substance use. This could be a favorite bar, drug paraphernalia, non-sober friends, etc.
- Overconfidence – After a short period of successful sobriety, a person may naïvely believe that they have “beaten” their addiction. But when they stop doing the right things and working their recovery program, they jeopardize everything they have worked for.
- Mental illness – A person may attempt to “self-medicate” with alcohol or drugs to alleviate symptoms of untreated conditions such as anxiety, depression, PTSD, or bipolar disorder.
- Poor impulse control – Chronic substance abuse can have a long-term effect on the area of the brain responsible for controlling impulsivity. With abstinence, the brain slowly returns to normal, but until then, the person is extremely vulnerable.
- Impaired judgment – Similarly, the area of the brain associated with decision-making is also affected.
These last two factors highlight addiction’s impact on the brain and explain why people new to recovery are at greater risk of relapse. Two-thirds of all relapses happen within the first 90 days.
“We treat both addiction and co-occurring disorders and accept many health insurance plans. Take a look at our outpatient program today!”
Recognizing Who is Most At-Risk
“We can improve our tailoring of treatment to each patient if we know who among patients…is at high risk for opioid relapse. As well, health care providers can target more aggressive therapies to those at high risk.” ~ Drs. Zena Samaan and Michael G. DeGroote, McMaster University School of Medicine But there are other factors that can influence the likelihood of relapse. According to a 2016 study conducted by McMaster University:
- Age at initiation of use matters. – for every additional year of age at first misuse of opioids, the risk of relapse increases by 10%.
- IV opioid abusers have a more than doubled risk of relapse, compared to individuals who do not inject drugs.
- For each day that a benzodiazepine tranquilizer was used, in the preceding month, there is a 7% increase in the risk of relapse.
Interestingly, – the older a person is currently, the less likely they are to suffer a relapse.
How Stress Contributes to Relapse
“The choice to reach for the bottle or the drug again can be a stress-driven choice. New research shows that addicts suffer feelings of stress in their body as the previous fix wears off. The addiction actually creates more stress for you just before you go back at it again! The physical comfort combined with feeling down beguiles you into using again to calm yourself.” ~ Lynne Namka, Avoiding Relapse: Catching Your Inner Con Active addiction is a dysfunctional, chaotic existence filled with stress – relationship problems, money worries, legal difficulties, etc. Unfortunately, these issues don’t magically or immediately go away just because the person is in recovery. Things DO eventually get better, but not all at once. Here’s the thing – substance abuse becomes a double-edged sword. While on one hand, it contributes to added stress, addicts and alcoholics frequently turn to intoxicants for relief. This poor coping method becomes an unhealthy habit that remains during early recovery. In other words, until more positive habits are instilled, the person will still want to relieve their stress with alcohol or drugs. This is why top rehab programs spend a lot of time teaching stress reduction techniques and practicing healthy coping methods.
Toxic Shame and the Risk of Relapse
“The pain an alcoholic feels is the pain of self-loathing and humiliation…from loss of respect…from isolation and loneliness…from awareness that he is throwing away much of his uniqueness…from gradually throwing away his body and soul. That pain doesn’t just vanish when you walk away from the bottle.” ~ Scott Stevens, Every Silver Lining Has a Cloud: Relapse and the Symptoms of Sobriety In 2013, a study published in Clinical Psychological Science concluded that someone overwhelmed with shame because of their past drinking problems is more likely to relapse and suffer additional health problems. Exhibiting pronounced shame behaviors is a strong predictor of relapse within four months. In fact, a person who showed a “moderate” amount of body language indicating shame drank an average of 20 more drinks than someone who displayed no such signs. Shame is a distinct feeling of guilt. Guilt is a sense of remorse over one’s behavior. But shame is a negative feeling about one’s self. Dr. Jessica Tracy, with the University of British Columbia, says, “If you are prone to shame, it’s incredibly painful and is one of the worst emotions to experience. People hate it. And one way to [escape it] is to drink because it helps you get out of your head. When you feel shame, you feel that who you are as a person [is] bad, and there’s nowhere to go with that, there is no solution.” “Guilt is much better. With guilt, you did a bad thing, but you can fix it.”
Taking Sobriety for Granted
“…if we don’t keep our mind on our inability to control our use after we take that first drink or hit, don’t keep that knowledge foremost in our consciousness, no amount of time will serve as a seawall against the incessant tides of addiction.” ~ William Cope Moyers, Now What?: An Insider’s Guide to Addiction and Recovery After months or even years of uncontrollable substance abuse, a person can feel a sense of accomplishment once they have achieved a period of sobriety. But with this stability can also come a degree of overconfidence. A person can feel that they have “beaten” their addiction. They may let their guard down and stop working their recovery plan. This can have disastrous results, especially in early recovery. Most addiction specialists agree that the length of uninterrupted time spent in a recovery program directly affects the likelihood of successful and lasting sobriety. This is particularly true early on.
- According to an article in the Los Angeles Times, 35% of people who are in alcohol or drug treatment for less than 90 days will relapse within, in comparison to just 17% of those who remain for 90 days or more.
- In a different study, individuals who leave treatment before 90 days relapse at a rate that is comparable to those who only stay in treatment for a few days.
- Only about a third of those who are able to abstain from intoxicants for less than one year will be able to stay abstinent.
- But among those who reach one year of sobriety, less than half will relapse.
“We accept many health insurance plans. You can get your life back in order with our outpatient program today!”
How to Prevent Relapse
“You may have to fight a battle more than once to win it.” ~ Margaret Thatcher The biggest way to prevent relapse is to earnestly work your recovery program:
- Attend all counseling and therapy sessions
- Actively participate in group sessions
- Communicate with your counselors
- Take anti-craving medications as prescribed
- Read recovery literature
- Do all homework and assigned exercises
- Meditate
- Practice stress reduction
- Go to 12 Step meetings
- Work with a Sponsor
- Eat properly
- Get plenty of rest
- Engage in positive self-talk
- Avoid triggers
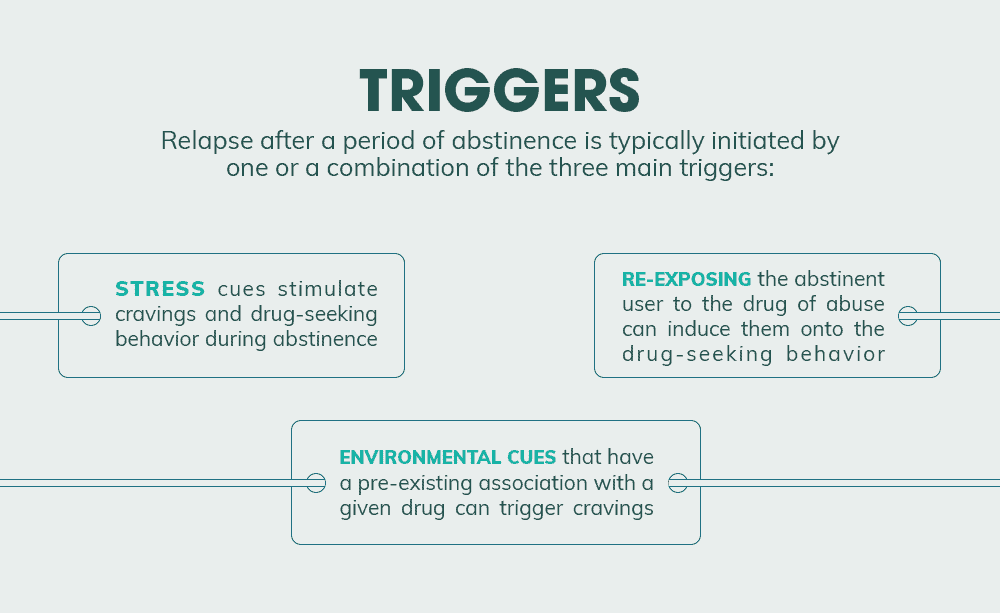
Avoiding Relapse Triggers
“A particular song, smell, or place can trigger memories that a person hasn’t thought of for years. The brain is very powerful, and potentially life-threatening triggers should not be taken lightly. Socializing with people who drink and use drugs can be a trigger. Going to a bar, with all of its familiar sights, sounds, and smells, can be a trigger. Mirrors, razor blades, rolling papers, certain music—any or all of these things—can trigger a relapse.” ~ Joe and Judy Herzanek and Karen Steenekamp,Why Don’t They JUST QUIT?: Hope for Families Struggling with Addiction “Triggers” are anything that can remind a person of substance use and make them feel the urge to start up again. They can be external, caused by experiences, or internal, caused by thoughts and emotions. External triggers:
- People – family and friends who still drink or use drugs
- Places – liquor stores, bars, nightclubs, certain neighborhoods, any place where you regularly used substances, etc.
- Things – drug paraphernalia such as needles, pipes, razor blades, rolling papers, commercials or movies featuring drinking or drug use, the smell of alcohol, etc.
One of the first lessons learned in early recovery is the necessity of staying away from these external triggers. It may be necessary to change your daily route, clean your home from top to bottom, or even find a whole new group of friends. Internal Triggers:
- Anxiety
- Depression
- Boredom
- Anger
- Frustration
- Loneliness
- Shame
To avoid these negative emotions that can lead to relapse, people in recovery are taught to practice mindfulness meditation, stay busy with positive activities, and work at using self-affirmation to build self-esteem.
Medications That Can Help
“With the current trend and national eye on addiction, more professionals are specializing in this type of care, called Medication-Assisted Treatment (MAT). MAT embraces behavioral therapy in conjunction with medicines for cravings, relapse prevention, and overdose production.” ~ Dr. Arwen Podesta, M.D. MAT is considered the most effective strategy that can support recovery from addiction. FDA-approved medications can ease cravings, alleviate anxiety, reduce withdrawal symptoms, stabilize moods, and help with insomnia. With MAT, up to 70% of patients are able to remain drug- and alcohol-free for at least a year. There are over two dozen medications that can provide these benefits:
- Acamprosate
- Baclofen
- Benzodiazepines
- Buprenorphine
- Buprenorphine/Naloxone
- Bupropion
- Buspirone
- Calcium Carbamide
- Carbamazepine
- Dextroamphetamine
- Disulfiram
- Gabapentin
- Methadone
- Methylphenidate
- Mirtazapine
- Modafinil
- Nalmefene
- Naloxone
- Naltrexone
- Nicotine
- Phenobarbital
- Propranolol
- Rivastigmine
- Tiagabine
- Topiramate
- Varenicline
While all of the above medications help with cravings, there are other prescription medications that can ease withdrawal symptoms:
- Clonidine
- Chlorpromazine
- Folic Acid
- Haloperidol
- Imipramine
- Methocarbamol
- Pregabalin
- Pyridoxine
- Thiamine
There are two caveats – be especially wary of accepting a prescription for any benzodiazepine-class medication. These drugs are highly habit-forming, even when taken as directed. 30% of all overdose drug deaths involve “benzos”. Additionally, ALWAYS have an open conversation with your doctor before taking ANY new medication.
Creating a Relapse Prevention Plan
“One of the most frustrating stages of recovering your health is when you realize you can do many things to help yourself stay well but you can’t figure out a way to do them regularly. It’s easy to forget simple things that you know, especially when you are under stress or when your symptoms are beginning to flare up.” ~ the Substance Abuse and Mental Health Services Administration You might accurately say that the entire recovery process is about preventing relapse. But after long-term substance abuse, successfully regaining your sobriety doesn’t just happen. Obviously, it takes a lot of time and effort, but making the necessary lifestyle changes to support recovery also involves dedicated adherence to a plan. Some people refer to recovery as a “sober journey”. Look at it this way – it’s hard to get where you want to go without a map. A relapse prevention plan IS that map. At its simplest, your rehab prevention plan is nothing more than answering a series of questions.
- How are you handling practical matters?
- Living arrangements
- Transportation
- Employment
When the necessities are taken care of, you eliminate unnecessary stress.
- What is your personal support system?
- Family members
- Friends
- Significant other
- Coworkers
- Professional counselors/Rehab program
- 12-Step Programs – Alcoholics Anonymous, Narcotics Anonymous, Celebrate Recovery
- Sponsor
Having support from others gives you a valuable resource when you are feeling overwhelmed or tempted.
- How much time are you devoting to recovery and mental health every week?
- Rehab requirements (day, evening, or outpatient sessions)
- Individual counseling
- Group therapy
- Mental health appointments
- Couples or family counseling
- 12-Step meetings (90 meetings in the first 90 days of sobriety is strongly recommended)
- Reading recovery literature
- Journaling
- Meditation/Prayer
In a very real way, your recovery IS your job now. It must become your first priority.
- What positive social/recreational activities will you engage in?
- Spending time with family and friends
- Dating (It is advised that you make no major relationship changes for the first year of sobriety)
- Hobbies
- Classes
- Outings
- Trying new things
Boredom is the enemy of recovery. Once upon a time, all of your time was spent finding, using, and recovering from intoxicants. Now, you can use all of this newfound free time to build a positive, sober life.
- How will you improve your relationships?
- Personal responsibility
- Apologies
- Amends
- Counseling
- Honesty
- Communication
- Can you name any lifestyle changes you have made/need to make to support your sobriety?
EXAMPLES: Avoiding friends and family members who still drink and use drugs Finding a new place to live Practicing scrupulous honesty Adopting a healthier diet Exercising regularly
- Now that you are sober, what are some realistic—and measurable—short-term goals you can work towards?
EXAMPLES: If unemployed, finding a job. If staying with family or a friend, moving into your own place. If CPS was involved, getting your kids back. Totally cleaning and redecorating your home to remove all substances and to celebrate your new life.
- What situations might put your sobriety in jeopardy?
EXAMPLES: Unhealthy relationships Unsafe environments Barriers to treatment No access to medication Untreated mental health issues
- In the situations you envision, what steps can you take to improve these?
EXAMPLES: Distance yourself Move, stay with friends, or go to a shelter Talk to your treatment team to find options Insurance, local assistance programs Get in touch with a qualified therapist If you are already participating in an alcohol or drug rehab program, then your treatment team is your best resource. Whatever your difficulty is, talk with them about it. They will have the experience and information you need to determine your best course of action.
The Stages of Relapse
“Relapse isn’t random…It’s usually a sign that a recovery program is lacking something. Most people who relapse can point to exactly what was missing and describe quite incisively how they slipped back into drinking or drugging. The signs and symptoms of relapse are well-established.” ~ Debra Jay, It Takes a Family: A Cooperative Approach to Lasting Sobriety Part of any good relapse prevention plan is vigilance against an impending relapse. Typically, a return to active substance abuse doesn’t happen all at once. There are progressive stages that move the person from recovery and sobriety to a full-blown relapse. While there is some overlap and the delineations between the stages aren’t always distinct, if you are watchful, you will be able to notice when your sober journey is starting to veer off course.
Stage I: Emotional Relapse
This first stage is not always deliberate. Some of the negative emotions that increase the likelihood of relapse include:
- Anxiety
- Agitation
- Frustration
- Extreme impatience
- Irritability
- Intolerance
- Blaming others
- Anger
- Sadness
- Depression
- Lack of gratitude
- Social withdrawal and isolation
- Mood Swings
- Self-neglect – poor personal hygiene, sleep disruption, unhealthy eating
Early recognition such emotional triggers can mean the difference between continued sobriety and a slip or relapse.
Stage II: Mental Relapse
In this second stage, the addict is often actively wrestling with both sides.
- They WANT to drink/use – Something or someone has triggered cravings.
- They DON’T want to drink/use – They know it’s a bad idea that could tear down everything they’ve built.
As with emotional relapse, there are a number of behavioral red flags:
- Glamorizing the past – “It wasn’t that bad.”
- Not going to 12-Step meetings or working the prescribed treatment plan.
- Justifying a “theoretical” relapse – “If I ever decide to get drunk again, here’s why…”
- Practicing dishonesty – Lying, stealing, cheating, etc.
- Engaging in risky behaviors
This is where a relapse prevention plan that includes a strong support system could safeguard recovery. NOW is the time to call for help.
Stage III: Physical Relapse
This third stage is marked by a return to active drinking and drugging. A relapse can last for a day or, tragically, for the rest of a person’s life. Here’s the thing – a relapse DOESN’T always mean returning to the former drug of choice. ANY attempt to become intoxicated – with ANY substance – is a physical relapse. This includes drinking alcohol, using illicit drugs, huffing inhalants, and misusing prescription medications.
Learning from Relapse
“The longer we stay sober, the more we need to know to maintain a sense of meaning, purpose, and comfort… the recovery process forces us to keep growing, learning, and changing.” ~ Terence T. Gorski, Passages through Recovery: An Action Plan for Preventing Relapse Despite all of your willpower, good intentions, and preparations, the insidious nature of addiction still makes a relapse a very real hazard. This is why one of the best things you can do to protect your progress in recovery is to also develop a relapse response plan. Different from a prevention plan, this is enacted after a relapse, in an attempt to:
- Involve members of the personal support system
- Determine what triggered the relapse
- Reevaluate the situation
- Determine any adjustments to the treatment plan
- Re-instill hope and lay the foundation for a return to treatment
At this low point, you may not be ready to immediately return to your recovery program, but that is precisely why your personal support system should be notified. They are there to reassure you that you are not alone, and that help is still available. They can assist you in assessing the situation and finding your way forward. It may seem difficult, but one of your key tasks after relapse is to stay positive. It was the disease of addiction that caused the relapse, not any moral or spiritual defect on your part. The sooner you acknowledge that, the sooner you can stop self-blaming and start recovery again, hopefully, picking up near where you left off.
Does Relapse Mean Recovery Has Failed?
“It is normal and natural to periodically get stuck on the road to recovery. It is not whether you get stuck that determines success or failure, but it is how you cope with the stuck point that counts.” ~ Terence T. Gorski, Passages Through Recovery: An Action Plan for Preventing Relapse OF COURSE NOT. When a relapse occurs, some people are far too quick to either point their fingers and assign blame or throw up their hands and give up completely. Both of those reactions ignore virtually everything we know about the disease of addiction. Look at hypertension, another chronic, yet manageable condition. Approximately 65 million people in the United States have high blood pressure. That is more than two and a half times the number of Americans who meet the criteria for a medical diagnosis of Substance Use Disorder. Like an addiction, hypertension is partly caused by genetics and partly by personal habits. Also like SUD, high blood pressure can be effectively managed with lifestyle changes – diet, exercise, weight loss – and medication. But when someone goes in for their annual checkup and they have not followed their doctor’s advice about self-care, no one stigmatizes them. It doesn’t matter if they’re 50 pounds overweight, binge on salty fried foods, and smoke three packs of cigarettes a day. No matter what the numbers are, their doctor might admonish them gently, stress the importance of habits, offer some educational resources, and then adjust their prescriptions. NO ONE accuses that patient of being morally deficient, lacking in willpower, or undeserving of a return to health, as they do with relapsing substance abusers. To a more imperative degree, this is how a relapse should be viewed – not as a time to “punish” the addict for their shortcomings, but rather, as an opportunity to review the treatment plan and make adjustments. Perhaps the only thing needed is a rededication to or a refocusing on the treatment plan that already exists. Maybe the treatment plan really is inadequate, and additional services are required. A different anti-craving medication might help. There is ALWAYS something else to be done. Consider heroin addiction: Heroin is considered to be the most-addictive drug on the planet, so much so that 1 out every 4 people who even try the drug develop a problematic use disorder. Once ensnared, nearly 80% of heroin addicts will relapse an average of 8 to 10 times before they are able to maintain their sobriety. But they ARE eventually able to recover. What is the takeaway? NEVER give on recovery.
What Did you Think About This Blog?
Give it a Rating!